Pressure Sore Prevention and Care
Pressure sores can also be known as bed sores or pressure ulcers. They are injuries to the skin and underlying tissues caused by sustained pressure.
Pressure related skin issues could happen to anyone if enough pressure is applied to the skin for a long enough period of time, however it is typically people who have increased care needs who are at risk.
Hospital patients, wheelchair users and people with poor mobility all fall in to the higher risk category for pressure sores. Conditions such as neuropathy and poor circulation can also raise the risk of developing a pressure ulcer.
How are pressure sores caused?
As mentioned in the introduction, pressure sores are developed by long periods of applied pressure to parts of the body.
The applied pressure denies the skin and other tissues of the blood flow needed. Lack of blood flow can lead to tissue damage and a wound developing.
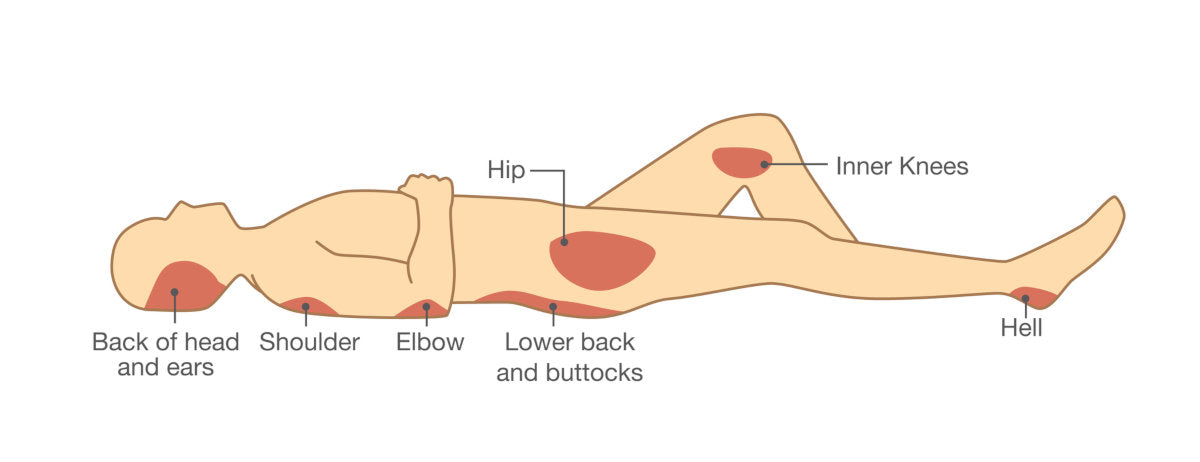
Common areas for pressure sores are where bony prominences are in contact with a surface for long periods of time:
- Head and Ears
- Shoulder
- Elbows
- Buttocks / Sacrum
- Insides of the Knees
- Heels
Looking at all the body parts which are typically affected you can see how this would relate to someone in a hospital bed, wheelchair or someone who has difficulty changing their position themselves.
Conditions with a Higher Risk of Developing Pressure Sores
Anybody can develop pressure ulcers but these groups of people have a greater risk of development:
- Poor General Health and Diet
- Increased Age – Typically Over 70 – due to reduced mobility and other health complications
- Being Overweight / Obese
- Incontinence
- Post-Surgery / Long Hospital Attendances
- Medical Problems which Reduce Mobility or Circulation – Respiratory Disorders, Diabetes, Parkinson ’s Disease, Multiple Sclerosis.
Signs of Pressure Sores

If you care for someone that has reduced mobility or spends a long time in their bed it is important to look out for early signs such as changes in colour of the skin developing in small patches near to bony prominences. The skin may feel warm, hard or spongy and when pressing it may not turn white. Pain is also a great indicator of a pressure sore developing.
Advanced symptoms of pressure sores are open wounds and infection and they are categorised depending on their severity. Worst case scenarios can involve the injury affecting multiple layers of tissue which can expose bone – this is only in more severe and advanced cases.
Management of pressure sores at this stage depends on severity but nursing care, medication and wound management may be required in order for the sore to recover properly.
If you see red swollen skin, signs of infection such as pus, high pain levels and with the addition of a temperature or other symptoms – you should seek urgent medical help.
Pressure Sore Prevention
Treatment for a pressure sore should obviously be avoided at all cost and preventing them in the first place is the best answer.
Here are some key points for preventing pressure sores:
1. Regular Movement
this is king over all other preventative measures as lack of movement and static positions is the main cause. Be mindful; of your position or the person you are caring for and ensure you’re moving regularly, especially from pressure points.
2. Use of Pressure Care Equipment
Use of pressure care equipment for wheelchairs, beds and even clothing to help reduce the chances of developing pressure sores. Typical seat cushions and mattresses are designed with a solid surface, whereas pressure care versions are made up of spaced padding which aids reducing surface pressure. The Roho Mosaic Cushion is popular with wheelchair users for example.
For areas such as the feet, elbow, heels and ankles, there are special padded shoes and slippers which can help – these can be particularly good with people who suffer poor circulation to their lower limbs and are at risk of ulcers.
Medical sheepskin has been proven to be helpful in the management of pressure sores,
3. Being as healthy as you can be
Eating a good varied diet to aid repair of the body and general health can help your body heal quicker. Not smoking can help to improve your circulation and again help to promote better healing.
4. Risk Assessment
A thorough risk assessment of the person you care for should always be done and the team that are managing the person should be made aware of. Take in to account their mobility, current health and any medical issues they have.
This is a basic guide to pressure sores – as stated before, if you have suspicion of pressure sore development, contacting a medical specialist should be a first port of call.
If you have found this article helpful and you think someone could benefit from this, please share it. If you have any pressure care product questions, please contact Breeze Mobility and we will be happy to answer any of your questions.

